Most people who suffer from severe headaches don’t think about going to the dentist to get help. But a dentist may be the right professional to turn to if you physician has not been able to determine the root cause of your pain. But first it’s important to determine whether the headaches you are experiencing fit into the primary or secondary category.
Primary headaches are migraines, tension headaches and cluster headaches. Many dentists do see patients with primary headache problems, but it’s the for the secondary type of headache that they can be particularly effective.
So, Can A Dentist Cure Your Headaches?
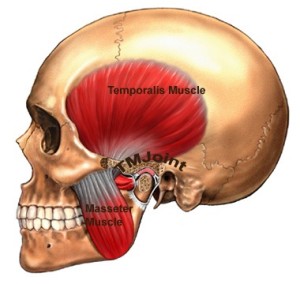
Secondary headaches can be caused by many things, but in particular trauma to the temporomandibular joint, the joint of the jaw. This is frequently referred to as the TMJ. A traumatized TMJ can be the result of injury, a structural deficiency, a malocclusion (bad bite), newly placed or worn dental work, oral disease, or sleep bruxism (teeth grinding and clenching at night).
Many dentists today are trained in assessing and treating these kinds of pain problems (called orofacial pain) and while a dentist may not be able to cure your headache he or she can often discover the root cause. Dentists training in this special field are becoming increasingly important health team members in the diagnosis and treatment of the type of severe and persistent headaches that are TMJ-related.
If you clench or grind your teeth at night you are not alone. Millions of Americans do it. So, how does sleep bruxism often cause such severe headaches? Here’s how: the constant pressure is being exerted by the act of clenching and grinding your teeth can result in trauma to your TMJ. Next, the nerves become agitated and here comes the pain. But what’s tricky is this is that pain from the TMJ can show up in other places on your body, such as your neck, your face, or even your head. This is called referred pain. Your TM joints are positioned very close to your cranial nerves, and severe headaches are often the result.
Do all the pieces now fit into place? If yes, find a dentist who is trained in treating orofacial pain problems. The best practitioners will not only be able to determine the source of your pain, but will put a treatment plan in place that include massage, relaxation techniques, a nightguard to protect your teeth, or even Botox.
I’ve been treating patients with this very same problem for over 30 years, and in most cases, with a change in lifestyle to reduce bruxism combined with treatment, the outcomes are very positive.
Start by asking your physician for a referral to a dentist with orofacial training or check out AAOP which is an organization dedicated to providing referrals and support for suffering headache patients like you. Good luck!