Last week a 44-year old woman came in to see me concerned with the fact that the her face had become more and more “square-shaped” over the past ten years. She openly revealed that working full time and raising three kids had been no easy task for her and that she often went through the entire day with her teeth clenched. I explained to her that those ten years of teeth clenching had essentially been causing her to make a “fist in her face” for all those years. With that kind of daily stress on the muscles, it’s no wonder that her face had changed!
The end result of her clenching behavior was that she had “buffed” her jaw muscles. They bulged outwardly just like your biceps would as a result of lifting weights every day over a prolonged period of time. Remarkably, my patient never experienced any pain in her face or her jaws, which probably would have caused her to seek help sooner. The issue for her now, however, was the change in her appearance.
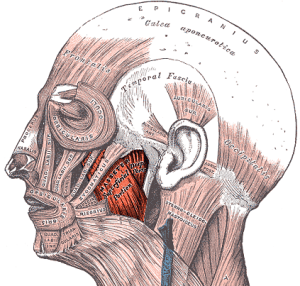 My examination (not surprisingly) revealed that she had bulky and powerful jaw muscles (masseter) that bulged outwardly when her teeth were clenched together. Even the muscles in her temples bulged! Over the decade this patient had actually increased the size and number of muscle fibers giving her a ‘Clint Eastwood’ look.
My examination (not surprisingly) revealed that she had bulky and powerful jaw muscles (masseter) that bulged outwardly when her teeth were clenched together. Even the muscles in her temples bulged! Over the decade this patient had actually increased the size and number of muscle fibers giving her a ‘Clint Eastwood’ look.
The first hurdle in treatment was to get the patient to actually change her acquired behavior and learn to live in the world with her teeth apart during the day. The clenching tendency that she had developed was likely the result of trying to cope with her daily stresses, some of which were not under her control. Relaxation and breathing techniques were reviewed, and she began to use an oral appliance during the day to create awareness. This was the first part of the plan. As experience has taught me, just stopping new muscle building does not effectively reduce the bulk of jaw muscles in a predictable fashion. Once built, these muscles tend to stay large as a result of normal daily activities. So what next?
Botox Injections:
In order to actually decrease the size of her well-built muscles, we needed to reduce the ability of these muscles to contract forcefully on a day-to-day basis. This is where Botox can really help. We administered three Botox injections into the patient’s masseter muscles; each injection session approximately three months apart. With time, the Botox led to muscle atrophy (size reduction and less strength) without compromise of eating or talking along the way. The result was a return to a more normal jaw profile.
To assure a lasting result my patient has to continue participating. This means teeth apart during the day and wearing the bite plate appliance at night (to diminish the impact of her night clenching). Some simple jaw stretching exercises are also required to keep the jaw muscles supple.
Although it took almost one full year from start to finish, this cosmetic makeover has truly made a difference in slimming my patients’ facial profile that was the end result of years of muscle building. This is probably the only time that reducing muscle bulk actually can make someone look better!



 Amidst the commonly used therapies to address
Amidst the commonly used therapies to address 
 Over the past year in my practice we have seen an increasingly number of female patients who are committed fans of high intensity indoor cycling workouts (sometimes called “spinning”) such as Soul Cycle. They have been arriving complaining of jaw pain, limited jaw motion, and jaw clicking, all the typical signs of
Over the past year in my practice we have seen an increasingly number of female patients who are committed fans of high intensity indoor cycling workouts (sometimes called “spinning”) such as Soul Cycle. They have been arriving complaining of jaw pain, limited jaw motion, and jaw clicking, all the typical signs of