Do you suffer from TMJ symptoms, jaw pain, or both? As a TMJ doctor, I have many tools at my disposal for my patients who suffer from tight, painful jaw muscles. To help them feel better I recommend at-home treatments for TMJ that work really well. I want to share some of them with you.
Over the years I’ve recommended (and developed) a number of relaxation techniques and massages for TMJ and jaw muscle pain. If you notice yourself opening and closing your mouth all day long to stretch out your jaw muscles, you probably have a TMJ problem. Try some of these to get some relief.
TMJ Relaxation Techniques and Breathing Exercises
Most people with ongoing jaw pain and tightness tend to breathe with shallow chest movements during the day. As a matter of fact, if you suffer from any kind of muscle pain you probably breathe too quickly. This results in an imbalance of the oxygen and carbon dioxide in your body and sets you up for more even muscle pain and fatigue.
The following techniques will help you slow your breathing (most of us take too many breaths per minute) and help your muscles to relax:
With your lips lightly touching, place your tongue gently on the roof of your mouth behind your front teeth, or place your tongue gently against the back of your lower front teeth. Then, bring air in through your nose and extend your belly outward. Hold this for 3 seconds and then exhale through your mouth while parting your lips slightly. Repeat 6 times. You can do this once every hour.
Try this as well: With your lips lightly touching and your tongue gently placed against your lower front teeth or your upper front teeth (or just floating in no particular position) breathe in through your nose for 4 seconds (fill your belly). Then, exhale through your lips or nose for 4 seconds. Pause for 2 seconds. This entire process should take only 10 seconds. Repeat this 6 times over a 1-minute period. This will help you train yourself to slow down your breathing. Perform this once every hour whenever you need it.
Massage for TMJ and Sore Jaw Muscles
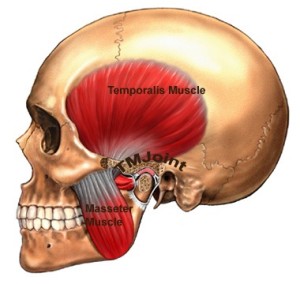
A sore jaw indicates that your muscle health has been compromised and is likely due to the accumulation of an irritating substance which forms in response to muscle overuse, such as lactic acid. The key here is to increase the blood flow to those sore muscles which in turn brings fresh oxygen and nutrients to the affected area. The Temporalis and the Masseter are the two most important muscles for you to focus on.
Using your index and your middle finger massage the sore areas in each of these muscles in a circular motion for 6 seconds on the right side, and 6 second on the left. If you can, do both sides simultaneously. Perform this massage with your mouth hanging slightly open, and your head relaxed. Press firmly, but not so hard that tears come to your eyes. After massaging the muscles, open your mouth to its fullest non-painful position and then close your mouth slowly. Repeat this 6 times.
There are muscles inside your mouth that also can benefit from gentle massage. I find this one is best done in the shower. Open your mouth half way and place the pad of your index finger on the most rear upper tooth on one side. Then slide your index finger off that tooth moving toward the cheek in an upward direction. You should run into a wall of bone. That is where your jaw muscle attaches, and is likely to be very tender. Once you’ve found the tender region, push your index finger inward and hold for at least 30 seconds before releasing. Then switch to the other side and repeat. Massage each side 2 times.
(You can also move your index finger in a circular pattern instead of maintaining constant pressure.)
Exercises for Sore Jaws
This exercise is designed to release tension in the muscles that enable you to open and close your jaw jaw. Place your tongue as far back as possible on the roof of your mouth. Now, try to open your mouth, keeping your tongue in this position (the range of motion will be very limited). While your tongue remains in place, position your thumb under your chin and attempt to open your mouth against the resistance of your thumb. Maintain the resistance for 3 seconds before releasing. Repeat this 6 times. This exercise can be performed up to 6 times per day.
Here’s another technique that many of my patients find helpful. Blow air into your your cheek on one side and hold it for 6 seconds. Then switch to the other side and do the same thing. This can be done 6 times per day.
You can also do some tongue exercises to loosen tight jaw muscles. With your lips sealed, move your tongue in a complete circle 6 times to the right and then 6 times to the left. Then take 6 cleansing belly breaths as described above and repeat the tongue movements 2 more times.
Tight jaw muscles can produce serious pain. If you are suffering, try some of the above massages and exercises for a week or so and see if you feel better.
Please let me know which technqiue eases your pain the most.
Good Luck!
Dr. Donald Tanenbaum is a specialist with offices in New York City and Long Island, NY. He is uniquely qualified to diagnose and treat problems associated with facial pain, TMJ, headaches and sleep apnea.







 Over the past year in my practice we have seen an increasingly number of female patients who are committed fans of high intensity indoor cycling workouts (sometimes called “spinning”) such as Soul Cycle. They have been arriving complaining of jaw pain, limited jaw motion, and jaw clicking, all the typical signs of
Over the past year in my practice we have seen an increasingly number of female patients who are committed fans of high intensity indoor cycling workouts (sometimes called “spinning”) such as Soul Cycle. They have been arriving complaining of jaw pain, limited jaw motion, and jaw clicking, all the typical signs of